Endothelium Function in AS Improved with Methotrexate Alone or Combined with Anti-TNF Agents, Study Finds
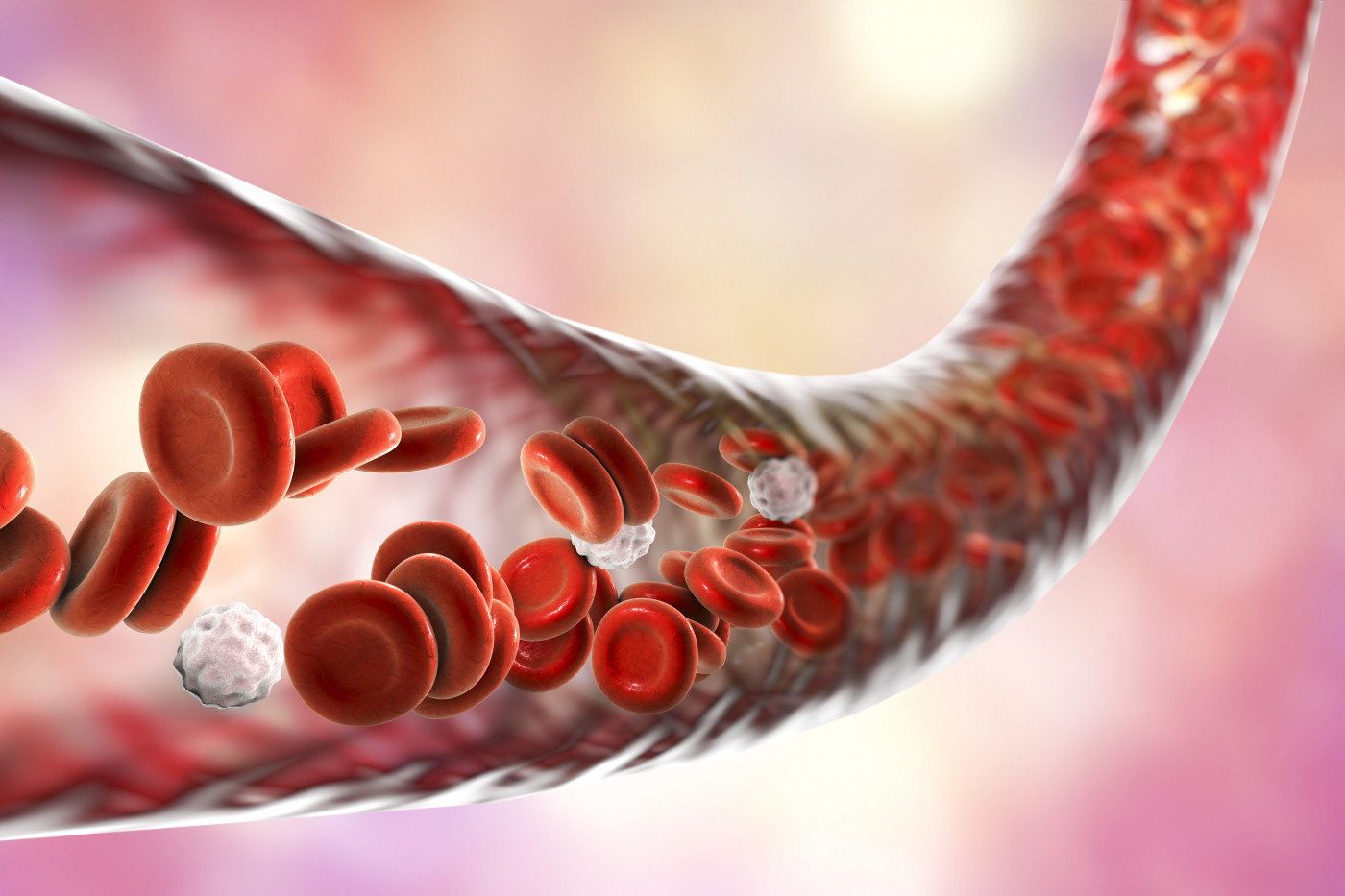
Methotrexate alone or combined with therapies targeting the inflammatory tumor necrosis factor (TNF) may help improve the endothelium function – the thin membrane that lines the inside of the heart and blood vessels – in patients with inflammatory arthritis.
The study, “Methotrexate and anti-tumor necrosis factor treatment improves endothelial function in patients with inflammatory arthritis,” was published in the journal Arthritis Research & Therapy.
The first feature characterizing the different forms of inflammatory arthritis – ankylosing spondylitis (AS), rheumatoid arthritis, and psoriatic arthritis – is dysfunction of the endothelium, which is characterized by reduced vasodilation, a pro-inflammatory state, and pro-thrombic properties, which refers to abnormal blood coagulation.
An improved endothelial dysfunction in patients with inflammatory arthritis is important because it is one of the first stages of atherosclerosis, a condition that can lead to cardiovascular disease. And the incidence of heart disease is higher in conditions associated with inflammatory arthritis.
Whether anti-rheumatic therapies – such as methotrexate (sold under the brand names Trexall and Rheumatrex, among others) and anti-TNF therapies such as Enbrel, Remicade or Humira – improve endothelium dysfunction in patients with AS and psoriatic arthritis remains largely unknown.
Researchers analyzed all patients with rheumatoid arthritis, AS, and psoriatic arthritis who participated in the PSARA observational study (NCT00902005), and were evaluated for endothelium dysfunction, a total of 113 patients. Sixty-four patients had rheumatoid arthritis, 29 had psoriatic arthritis, and 20 had ankylosing spondylitis.
Study participants received either a monotherapy of methotrexate or a combination of methotrexate and anti-TNF.
“We evaluated changes in the Reactive Hyperemic Index (RHI) after [six] weeks and [six] months of antirheumatic therapy,” researchers wrote. The RHI is an indicator of endothelial function.
The results showed that in all inflammatory arthritis patients with endothelium dysfunction, the RHI significantly improved after six weeks and again after six months of treatment. Comparing both types of treatment, the RHI of patients who received methotrexate monotherapy was better than in patients treated with methotrexate plus anti-TNF.
The fact that the effects were more pronounced with methotrexate monotherapy “might be due to a more sustained beneficial effect of MTX [methotrexate] on the vasculature,” the researchers wrote.
Looking at each diagnosis specifically, while apparently all groups showed improvements in RHI from baseline to six weeks after treatment and again at six months, this was only statistically significant in the group with rheumatoid arthritis.
Overall, these results suggest that treatment with methotrexate alone or combined with anti-TNF leads to an improvement of endothelium function, with methotrexate alone having a more pronounced effect.






