Satellite Rods Yield Good Outcome in ‘Humpback’ Surgery, Study Finds
Chinese researchers examine those with ankylosing spondylitis-related kyphosis
People with ankylosing spondylitis (AS)-related kyphosis — a “humpback” appearance — showed good post-surgery outcomes with a technique called satellite rods, a Chinese study shows.
The use of satellite rods had been linked to a lower rate of complications in people undergoing spinal surgery, but its use in AS-related kyphosis had not been reported.
The study, “Clinical Results of Utilizing the Satellite Rod Technique in Treating Ankylosing Spondylitis Kyphosis,” was published in the journal Orthopaedic Surgery.
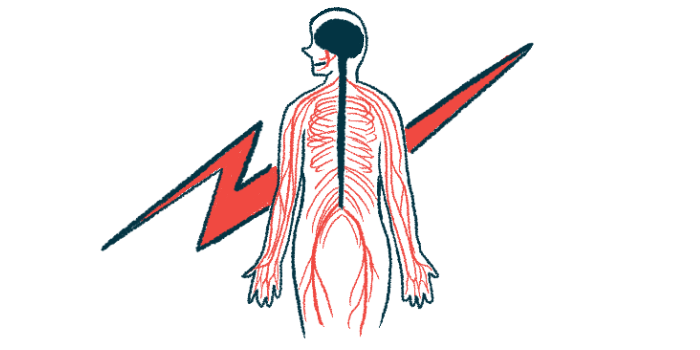
AS is a type of arthritis that affects the spine, often leading to deformities that may result in walking and standing impairments. AS kyphosis is characterized by an exaggerated, forward curvature of the upper back, leading to a “humpback” appearance.
In patients with severe AS kyphosis, surgery is used to reestablish the spine’s natural curvature — called sagittal balance — a key feature to maintain an upright, efficient, and painless posture.
Pedicle subtraction osteotomy (PSO) is a surgical procedure widely used for treating AS-related kyphosis. It consists in cutting out the pedicles — bone projections that stick out from the back part of the vertebra — of the targeted region. The spine is then realigned and stabilized by rods that hold it in position while it heals.
However, despite the satisfactory results with PSO, “complications of the procedures still need to be considered, especially failure of the rods,” the researchers noted.
While the risk of rod fracture is lower in patients with AS kyphosis when compared with people with other spine deformities, “rod fracture still cannot be ignored as a potential complication,” they added.
The use of “satellite” rods (a multirod construct not connected to the primary rods) was previously shown to reduce the risk of rod failure. However, “there are no clinical reports documenting the use of the satellite rod technique in the treatment of ankylosing spondylitis kyphosis.”
The study and its findings
In this study, a team of physicians in China compared the clinical outcomes of AS kyphosis patients who underwent a PSO with and without satellite rods. Patients were followed for at least two years.
In total, they reviewed the outcomes of 119 patients (112 men and seven women, mean age 39.89 years) with AS kyphosis who underwent surgery. Those without satellite rods were divided into one-level PSO (57 patients) and two-level PSOs (33 patients).
The satellite rod group (29 patients) had one-level PSO, which is a less complicated surgery than the two-level PSOs, used to correct more advanced kyphosis.
Patients were followed for a mean of 29.31 months (about 2.5 years). The results showed that all three groups had a significant lessening of spinal deformity. No significant differences were seen in the level of correction (called the osteotomy angle) between the one-level group and the satellite rod group, 39.78 degrees versus 42.23 degrees. Patients in the two-level group had a lower osteotomy angle of 28.85 degrees.
Health-related quality of life significantly improved in all patients following surgery, as measured by the Bath Ankylosing Spondylitis Functional Index (BASFI) and the Scoliosis Research Society outcomes instrument-22 (SRS-22).
The BASFI, a tool to determine the degree of functional limitation, is composed of a set of 10 questions, which are scored from zero (no limitation) to 10 (maximal limitation in function). Before surgery, the mean score was 4.82, and after surgery it dropped to 3.25.
The SRS-22 is a patient-filled questionnaire to assess the outcomes after spinal surgery, with each question scored from one to five (higher scores indicate better health status). SRS-22 scores increased from 48.68 (pre-surgery) to 83.22 (post-surgery).
“All the patients reported that they would like to recommend corrective surgery to other patients who had the same disease,” the researchers wrote.
Complications after surgery were seen in 13 patients (10.92%). Three patients experienced rod fracture in the one-level group. No rod fracture or screw failure was observed in the satellite rod group or the two-level group.
Overall, these findings suggest that “the satellite rod technique is also recommended for patients who undergo PSO osteotomy to correct ankylosing spondylitis kyphosis deformities,” the researchers concluded.