Altered Gut Microbiome Contributes to Inflammation in Ankylosing Spondylitis, Study Suggests
People with ankylosing spondylitis (AS) have an altered composition of microorganisms in their gut, leading to more bacteria that play a role in inflammation and AS progression, a new study reports.
The study, “Metagenomic profiling of the pro-inflammatory gut microbiota in ankylosing spondylitis,” was published in the Journal of Autoimmunity.
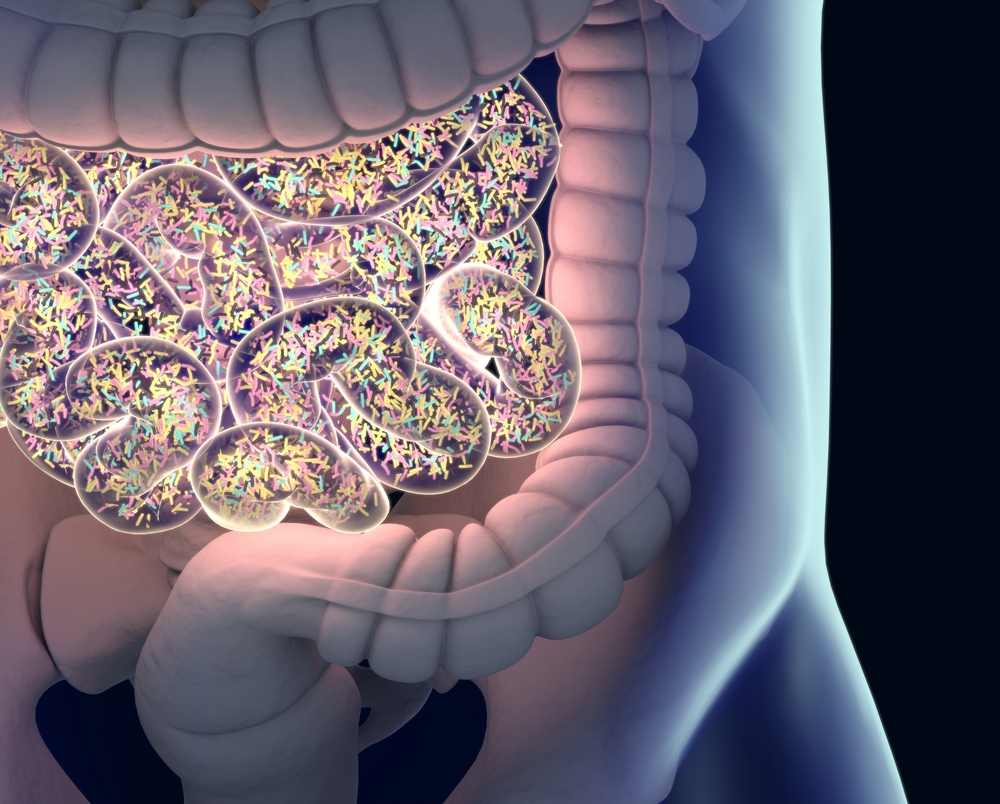
Trillions of microbes representing up to 1,000 different species colonize the human intestinal tract.
Studies have demonstrated that changes in the gut microbiome, which includes bacteria and fungi, are involved in multiple inflammatory diseases. In particular, imbalances in bacterial species have been linked with AS progression, but whether gut microbes cause the disorder remains unclear.
Researchers in China used an approach called “deep” sequencing to assess the fecal metagenome (all genetic material found in a sample) of the gut in people with AS.
The scientists analyzed the fecal metagenome of 108 people with AS — 85 untreated and 23 treated — and 62 healthy controls using a method known as metagenomic shotgun sequencing, which enables large-scale evaluation of bacterial diversity.
Results indicated that specific bacterial species, particularly Bacteroides coprophilus, Parabacteroides distasonis, Eubacterium siraeum, Acidaminococcus fermentans and Prevotella copri, were enriched in untreated AS patients compared to controls.
Interestingly, levels of Prevotella copri decreased in patients who underwent treatment. In contrast, some species that were reduced in people with AS, such as Enterococcus faecium, increased after treatment.
Subsequent analysis of affected pathways in AS patients showed increased oxidative phosphorylation (the major source of energy in cells), production of lipopolysaccharides (large molecules that are the main components of the cell wall of certain bacteria), and glycosaminoglycan degradation, which may lead to bone destruction and gut integrity damage.
Then, the team used a classification model to show that microbial signatures of the gut were highly accurate to diagnose AS.
Researchers also assessed the gut microbiome across different types of inflammatory arthritis. Besides AS, they used published metagenomics data of rheumatoid arthritis and Behcet’s disease (a rare disorder that causes blood vessel inflammation throughout the body).
In the three groups, the team found high levels of the bacterial species Bacteroides fragilis, Bilophila wadsworthia and Alistipes finegoldii, while Prevotella bivia and Eubacterium biformeand were depleted. Also, data from AS and rheumatoid arthritis showed a closer relationship than comparing either group with Behcet’s disease.
Reaction between auto-antigens (proteins that induce an abnormal immune response) and microbial components as causing autoimmunity — when the immune system attacks the body’s own healthy tissue — has long been suggested.
Using bioinformatics, researchers found three peptides (short protein sequences) among bacterial species enriched in AS patients that are similar to auto-antigens with a known role in AS.
One of these microbial peptides (known as “HIGQPGVIG” from Bacteroides fragilis) stimulated secretion of the pro-inflammatory molecule IFN-gamma by immune cells in AS patients, but not in controls.
This peptide mimics another peptide in type II collagen, the main component of cartilage, which is called molecular mimicry – the possibility that foreign peptides and the body’s own peptides share very similar sequences.
“Thus, it is rational to postulate that the autoantibodies triggered by the microbial peptide might aggravate AS progression by damaging the cartilage of inflammatory joints,” the scientists wrote.
“These findings collectively indicate that gut microbiota was perturbed in untreated AS patients with diagnostic potential, and some AS-enriched species might be triggers of autoimmunity by molecular mimicry,” they added.






