Hip, Knee Replacement Surgeries More Frequent in Older AS Patients than the General Population
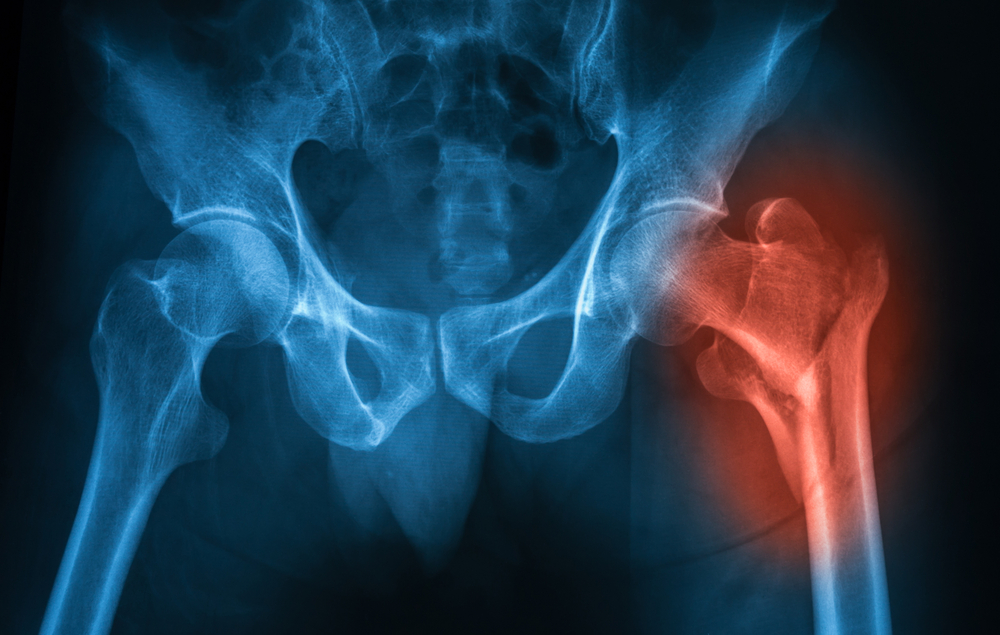
Total hip replacement surgery, or hip arthroplasty, has doubled in older patients with ankylosing spondylitis (AS), outpacing the rates in the general population over recent years, a U.S. population-based study shows.
AS patients who had this surgery had twice as many knee replacement interventions, compared to patients who did not have a hip surgery, drawing attention to the fact that hip replacement might be considered earlier to avoid further disability and damage to the knee, researchers say.
The study, “Increased Rates of Both Knee and Hip Arthroplasties in Older Patients with Ankylosing Spondylitis“, was published in the Journal of Rheumatology.
Ankylosing spondylitis (AS) is a type of arthritis that mainly affects the joints of the spine, causing inflammation of the spinal joints (vertebrae), leading to severe, chronic pain and discomfort. Other joints also can be involved, including in the hips, shoulders, ribs, heels, and small joints of the hands and feet.
Next to the spine, the hips are the second-most part of the body affected by AS. Studies indicate that up to 40% of AS patients report symptoms of hip arthritis, and 12% to 25% of those end up requiring a total hip replacement surgery, or arthroplasty after 30 years of living with the disease.
Total hip arthroplasty consists of surgically removing the damaged bone and cartilage and replacing it with an artificial joint (prosthesis).
For the past decade, rates of total hip arthroplasty have risen by 50% in the U.S. population overall. “These increases may be attributable in part to changing clinical indications and more liberal use of [total hip replacement],” the researchers wrote.
However, it is not clear whether the same trend has occurred in AS patients, given that clinical indications for total hip replacement surgery in these patients have not changed.
To investigate that, researchers used population-based data of U.S. Medicare beneficiaries to compare rates of total hip arthroplasty between older patients with AS and those without AS, and examined trends in these rates from 1999 and 2013. They analyzed data of 52,568 patients with AS (younger than 75 years, mean age 59 years) and 4,617,179 patients without AS (mean age 66), during that period.
They also examined how many patients had a total knee replacement. Knees usually are not affected in AS, but may be damaged secondary to longstanding hip arthritis. Hip contractures may develop and lead to knee contractures and altered gait. This, together with abnormal weight bearing, can result in knee damage requiring an arthroplasty.
From 1999 to 2013, AS patients always had more primary (meaning first-time) hip arthroplasties than the general population. In 1999, rates in the AS group were 4.6 per 1000 patient-years versus 1.9 in the control group. This means that in 1999, if we were to follow 1,000 AS patients over one year, there would be 4.6 patients receiving surgery.
Over the study period, the rates of total hip replacements among AS patients progressively rose, doubling from 4.5 to 9.6 per 1,000 patient-years, during the study period.
This showed that rates of total hip arthroplasty in older patients outpaced the increase in the general population, researchers say.
“Reasons for this increase are unclear but may reflect wider use of THA [total hip arthroplasty] among patients with AS after appreciation of acceptable frequencies of perioperative complications and good longterm outcomes,” the researchers wrote.
Knee arthroplasties outpaced hip replacement surgeries and also were more common among older patients with AS compared to the general population, in all years studied. For instance in 2013, knee arthroplasty rates in AS and non-AS subjects were 12.3 and 5.7 per 1,000 patient-years, respectively.
Moreover, the data revealed that patients who underwent a hip arthroplasty, had a knee replacement twice as often as those who did not need a hip arthroplasty — a rate of 20.4 versus 10.2 per 1,000 patient-years.
“The increased risk of TKA [total knee arthroplasty] in AS may be a consequence of damage from knee inflammation, or alterations in lower extremity biomechanics due to hip arthritis,” the researchers explained, adding this also raises questions about the right time to get a hip replacement.
“THA is often postponed in younger patients with AS out of concern for the need for future revision hip arthroplasties. This strategy may need to be reconsidered if postponement of THA not only prolongs pain and disability, but also results in greater secondary knee damage and a need for TKA in the future,” they concluded.






