Ankylosing Spondylitis Patients Have Different Biodiversity in Gut, Study Finds
Patients with ankylosing spondylitis have differences in the diversity of the fungi and bacterial populations that reside in the gut compared with healthy individuals, a study shows.
The study, “Altered Bacteria-Fungi Inter-Kingdom Network in Gut of Ankylosing Spondylitis Patients,” was published in the journal bioRxiv.
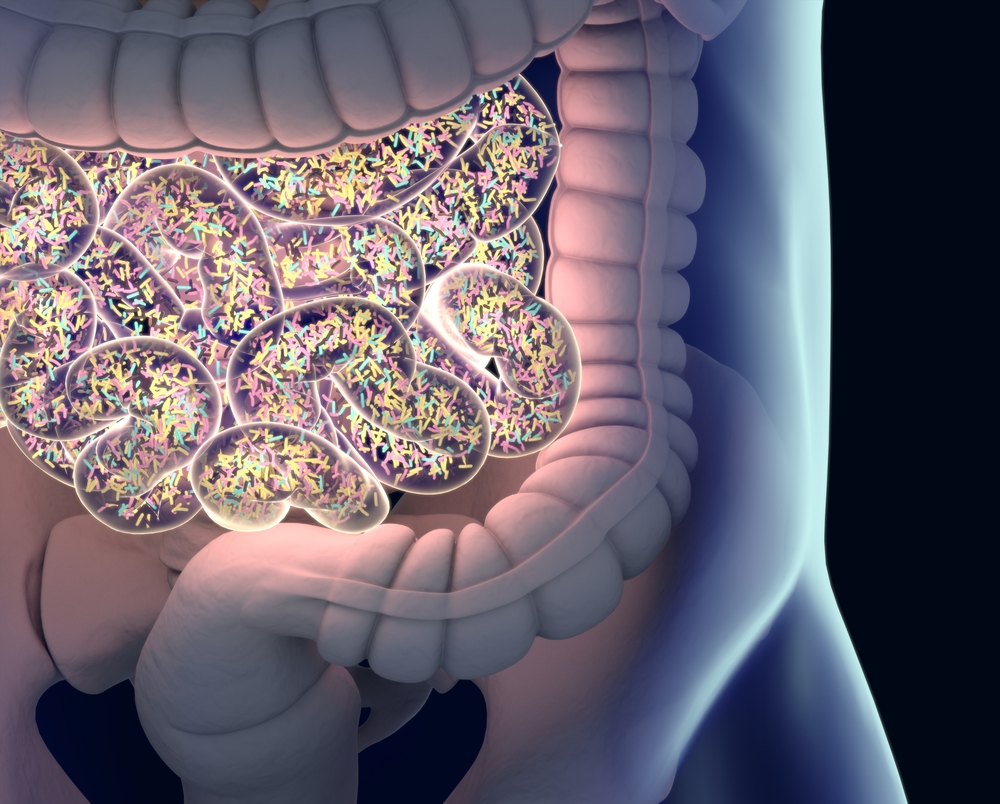
While the exact cause of ankylosing spondylitis is not known, studies have increasingly shown altered immune responses toward the gut microbiome influenced by genetic and environmental factors in autoimmune diseases related to ankylosing spondylitis. The gut microbiome refers to the population of microorganisms — such as bacteria and fungi — that inhabit the gut.
In fact, up to 70% of ankylosing spondylitis patients tend to have asymptomatic gut inflammation, and 5-10% of these patients develop severe intestinal inflammation that progresses to clinically defined inflammatory bowel disease (IBD), an autoimmune disease associated with chronic inflammation of the gut.
Because intestinal dysbiosis — which refers to the imbalance of the gut microbial population — is increasingly linked to IBD, researchers believe there is a close link between gut microbiota and ankylosing spondylitis development.
To study this, researchers in China characterized the bacterial and fungal populations in fecal samples from 22 ankylosing spondylitis patients and 16 healthy individuals, using high through-out sequencing. This technique looks for DNA sequences specific to different microorganisms in order to quantify their population in the gut.
Ankylosing spondylitis patients had a distinct pattern of fungi population, known as the mycobiota, as well as an imbalance (dysbiosis) of the bacterial population, known as the microbiota, compared with healthy controls.
The diversity of the fungi population was lower in ankylosing spondylitis patients, who also had a more significant imbalance of their mycobiota rather then their microbiota, compared with controls.
Specifically, the fungi population in ankylosing spondylitis patients consisted of higher levels of Ascomycota, which represents the largest fungi taxonomic group. Conversely, these patients had lower levels of Basidiomycota.
“The abundance of Ascomycota and Basidiomycota were strongly negatively correlated with each other and were among the most important discriminative features between [ankylosing spondylitis] and [healthy controls’] mycobiota,” the researchers wrote.
Interestingly, the Basidiomycota-to-Ascomycota abundance ratio is also different in IBD patients compared with healthy individuals, suggesting that the imbalance is either driven by, or involved in, the inflammatory process.
Researchers then compared gut microbiome differences between patients on different therapeutic regimens or who displayed different disease activities.
Some differences were found in the mycobiota of ankylosing spondylitis patients when grouped by different therapeutic regimens. Notably, treatment with biologics and non-steroidal anti-inflammatory drugs (NSAIDs) was associated with a lower abundance of fungal diversity than that in untreated patients.
Additionally, patients with varying levels of disease activity and radiographic damage had different patterns of mycobiota, suggesting the importance of mycobiota in disease progression.
“Our study identified a distinct mycobiota dysbiosis in [ankylosing spondylitis] in addition to the alterations in bacterial microbiota,” the researchers wrote.
“Further large scale investigations on the characterization of gut mycobiome in [ankylosing spondylitis] patients are needed to form a foundation for research into the relationship between mycobiota dysbiosis and [ankylosing spondylitis] development,” they concluded.






