Blocking IL-23 Not Sufficient to Treat Ankylosing Spondylitis, Phase 2 Trial Finds
Inhibiting IL-23, a molecule involved in inflammation, was not found to be clinically meaningful to treat ankylosing spondylitis, according to the results from a Phase 2 trial.
The study, “Risankizumab, an IL-23 inhibitor, for ankylosing spondylitis: results of a randomised, double-blind, placebo-controlled, proof-of-concept, dose-finding phase 2 study,” was published in the journal Annals of the Rheumatic Disease.
Ankylosing spondylitis (AS), a chronic inflammatory disease, is associated with back pain, progressive structural and functional impairment, and reduced quality of life.
AS patients do not generally respond to standard disease-modifying anti-rheumatic drugs (DMARDs). As such, there is a need for more biologic therapeutics, those that target individual molecules and tend to work faster than conventional DMARDs.
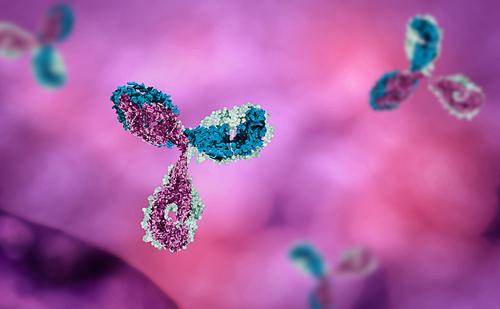
Recent studies have suggested that a molecule involved in immune inflammatory processes, called IL-23, may be targeted as a potential treatment strategy for AS.
AbbVie researchers have developed an antibody, risankizumab (BI 655066/ABBV-066), that can selectively inhibit IL-23. Risankizumab has been shown beneficial in other inflammatory diseases such as psoriasis, psoriatic arthritis (PsA), and Crohn’s disease.
Researchers conducted a Phase 2 (NCT02047110), proof-of-concept, dose-ranging study to determine the safety and effectiveness of risankizumab in AS patients.
A total of 159 patients with active disease were recruited and randomized to receive either a low (18 mg), medium (90 mg), or high (180 mg) dose of risankizumab or placebo over a 24-week period. Treatment or placebo was given at day 1 and weeks 8, 16, and 24.
The primary endpoint of the study was a 40% improvement in Assessment in SpondyloArthritis International Society (ASAS40) at week 12.
At week 12, all doses failed to reach the trial’s primary outcome of a 40% improvement in Assessment in SpondyloArthritis International Society (ASAS40).
ASAS40 evaluation determines the percentage of patients who achieved a 40% improvement in disease symptoms such as pain, inflammation, and physical function.
Specifically, the ASAS40 response rate for patients who received the low, medium and high dose of risankizumab was at 25.5%, 20.5% and 15.0%, respectively. Those in the placebo group had a ASAS40 response of 17.5%.
The estimated difference in the response rate between patients treated with the high dose risankizumab and placebo groups was –2.5%, suggesting there is no clinically significant improvement in patients treated with risankizumab.
In terms of safety, risankizumab was generally well tolerated and the rates of adverse events were similar across all treatment groups.
“Treatment with risankizumab did not meet the study primary endpoint and showed no evidence of clinically meaningful improvements compared with placebo in patients with active AS, suggesting that IL-23 may not be a relevant driver of disease pathogenesis and symptoms in AS,” researchers wrote.