Femoral Neck the Best Site to Measure Bone Loss in AS Patients, Swedish Study Finds
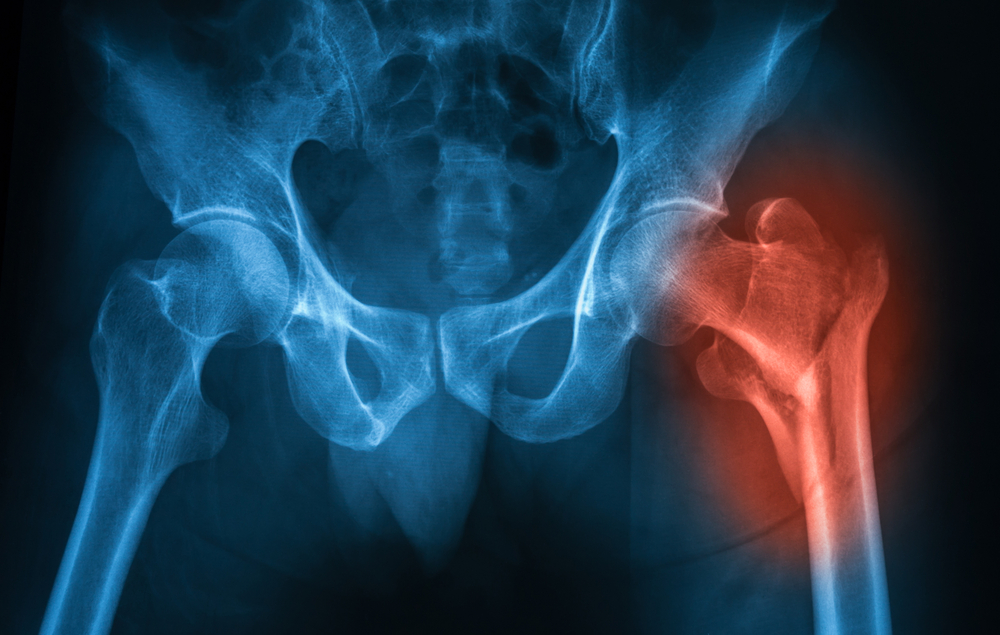
The best site to determine bone loss in ankylosing spondylitis (AS) patients is the femoral neck, according to Swedish researchers.
The study, “Which measuring site in ankylosing spondylitis is best to detect bone loss and what predicts the decline: results from a 5-year prospective study,” was published in the journal Arthritis Research & Therapy.
Patients with AS develop syndesmophytes (bone growth inside a spine ligament) and are at an increased risk for osteoporosis and vertebral fractures. Low bone mineral density (BMD) of the lumbar spine and the femoral neck has been reported in early and mild AS.
Bone mineral density is typically assessed by a technique called dual-energy X-ray absorptiometry (DXA). Measurements in the lumbar spine anterior-posterior projection – in which the X-ray enters the patient’s anterior side and exists posteriorly – are difficult to perform in AS due to calcifications over the vertebrae or to sclerosis of the vertebral endplates.
As a result, researchers hypothesize that lateral projection may be a better measuring site. “To our knowledge, no reports on changes over time in the lateral projection of the spine have been published,” the researchers wrote.
The team evaluated BMD changes over five years at different measuring sites in patients with ankylosing spondylitis to determine which is best for the diagnosis and monitoring of osteoporosis. They also analyzed disease-related variables and medication as predictors for osteoporosis.
A total of 204 AS patients with a mean age of 50 were recruited in 2009 from rheumatology clinics in Sweden. Bone mineral density was measured with DXA at the left hip (femoral neck and total hip), the lumbar spine – with anterior-posterior and lateral projections, and at the forearm (total radius). Measurements were conducted at baseline and after five years.
Questionnaires, blood samples, and spinal radiographs were also collected. AS-related alterations in the spine and vertebral fractures were assessed with standard scoring systems.
Of the initial 204 patients, 168 (82%, 92 men and 76 women) were re-examined after five years. BMD results showed decreases at the femoral neck and radius. But the result in the radius should be interpreted with caution given the high variability observed, the researchers said.
The data also showed BMD increases at the lumbar spine for both anterior-posterior and lateral projections. The result for anterior-posterior projections may be due to bone growth in the spine, the authors hypothesized. But the increase in lateral projection spinal BMD was surprising.
“Since we have no reference values for lateral BMD measurements for men, and since there is sparse knowledge in the literature how spinal lateral BMD changes over time in the general population, our results have to be interpreted with caution,” the researchers wrote.
Total hip BMD was also increased, particularly in younger patients with syndesmophytes.
The team noted that mean C-reactive protein levels – a standard marker for inflammation – during follow-up predicted a reduction in the bone mineral density of the femoral neck.
Conversely, the use of common osteoporosis medications like bisphosphonates predicted an increase in BMD at all measuring sites, except for the total radius. The use of tumor necrosis factor inhibitors (TNFi, which suppress the inflammatory response) also predicted an elevation in anterior-posterior spinal BMD.
Overall, the results “suggest that the best site to assess bone loss in AS patients is the femoral neck and that inflammation has an adverse effect,” the researchers wrote. Also, “the use of bisphosphonates and TNFi has a positive effect on BMD in AS patients.”
Future studies would benefit from including a control group and from having reference data for lateral projection, the team noted.