IL-17 inhibitors may help patients with CARD9 mutations: Early study
Mouse study implicates protein CARD9 in inflammatory cascade driving disease
People with ankylosing spondylitis (AS) who carry a mutation in the gene that encodes the CARD9 protein may be more likely to respond to treatments that block an inflammatory signaling molecule known as interleukin-17 (IL-17), a preclinical study suggests.
Scientists found that the protein CARD9 is involved in an inflammatory cascade that drives the disease in a mouse model. The protein does so by activating immune cells called neutrophils, which in turn activate other immune cells to trigger the production of IL-17.
The study, “Card9/neutrophil signalling axis promotes IL-17A-mediated ankylosing spondylitis,” was published in the Annals of the Rheumatic Diseases.
Signaling molecule IL-17 thought play key role in driving inflammation in AS
High levels of the inflammatory signaling molecule IL-17 are thought to play a key role in driving inflammation in AS, and some treatments, including Cosentyx (secukinumab) and Taltz (ixekizumab), work by blocking IL-17.
These therapies are effective for reducing disease activity in many, but not all, people with AS. In clinical practice, figuring out which patients are most likely to respond to IL-17-blocking treatments is largely a guessing game.
Mutations in the gene CARD9 (caspase recruitment domain-containing protein 9) have been linked with a heightened risk of developing AS. This gene provides instructions for making a protein, also called CARD9, which is known to play an important role in helping immune cells detect and destroy fungal infections.
Since mutations in the CARD9 gene can increase the risk of AS, it stands to reason that the CARD9 protein must have some biological function related to the development of the disease, but its exact function has been unknown.
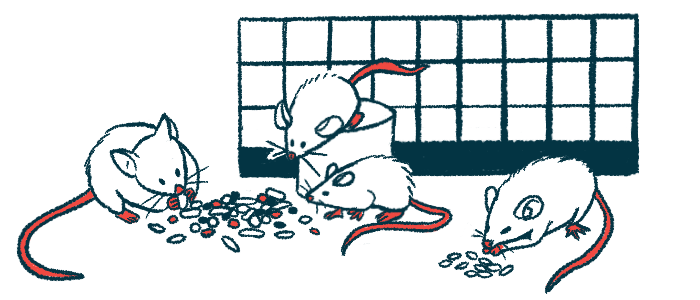
To learn more, scientists first conducted experiments in SKG mice, a mouse model characterized by IL-17-driven inflammation similar to what’s seen in people with AS.
This is the first time research has shown that we might be able to use genetic markers to determine which therapy ankylosing spondylitis patients should receive.
Mice lacking CARD9 had lower levels of IL-17, other inflammatory markers
The scientists reported that, when they engineered the mice so they could not produce any CARD9 protein, the SKG mice “showed little, to no signs of clinical disease.” Mice lacking CARD9 also had significantly lower levels of IL-17 and other inflammatory markers.
“Cumulatively, these findings indicate a role for Card9 in control over Th17-mediated disease in SKG mice,” the researchers wrote.
Th17 cells are the subset of immune T-cells mainly responsible for making IL-17. The researchers found that when they engineered mice to lack CARD9 in their T-cell precursors only, the mice could still develop AS, demonstrating that CARD9’s role in the disease is independent of the protein’s role inside of T-cells.
Instead, the scientists found that a lack of CARD9 leads to substantially reduced activation of another type of immune cell called neutrophils.
“Our data indicate a critical function for Card9 in controlling neutrophil responses during the induction of arthritis in SKG mice,” the scientists wrote.
Neutrophils are the “first responders” of the immune system to sites of infection or injury, but also can participate in the inflammation that drives AS and other autoimmune diseases.
The scientists found that when they engineered SKG mice to lack neutrophils, the mice had notably less severe disease and fewer Th17 cells, which is generally similar to what was seen in mice without CARD9. This implies that the main role of this protein in this disease model is to activate neutrophils, which in turn are needed to activate Th17 cells to make IL-17 and cause disease.
“Collectively, these data reveal a novel, neutrophil-intrinsic function of Card9 in directly potentiating neutrophil activation and IL-17A production by SKG T cells as the cellular mechanism by which Card9 drives arthritis in SKG mice,” the researchers wrote.
AS patients with more neutrophils tend to have more severe symptoms
The scientists also looked at data from people with AS collected by the U.S. Department of Veterans Affairs. They found a significant correlation between neutrophil counts and scores on the Bath Ankylosing Spondylitis Functional Index. In other words, the data suggested AS patients with more neutrophils tended to have more severe disease symptoms.
In lab experiments, the researchers found that neutrophils from people with more severe AS tended to provoke more IL-17 production from T-cells. Taken together, these data support the idea that abnormal neutrophil activity is an important driver of the disease.
The researchers also observed patients with a CARD9 mutation had significantly higher concentrations of the IL-17 protein in their blood compared to those with non-mutated CARD9 gene.
As such, patients with CARD9 gene mutations would likely be expected to respond to medications such as Cosentyx or Taltz. The scientists are currently working on additional research to test this hypothesis.
“This is the first time research has shown that we might be able to use genetic markers to determine which therapy ankylosing spondylitis patients should receive,” Ruth Napier, PhD, senior author of the study at Oregon Health and Science University, said in a press release.