S100A4 Protein Levels May Be Early Biomarker of Axial Spondyloarthritis, Study Suggests
Written by |
Blood levels of the protein S100A4 are elevated in patients with axial spondyloarthritis (axSpA), especially at early stages of the disease, a study found.
The excessive spinal bone formation that occurs over time seems to be marked by a reduction in the protein’s levels, suggesting its implication in the development of the disease, the researchers said.
The study, “S100A4 is elevated in axial spondyloarthritis: a potential link to disease severity,” was published in the journal BMC Rheumatology.
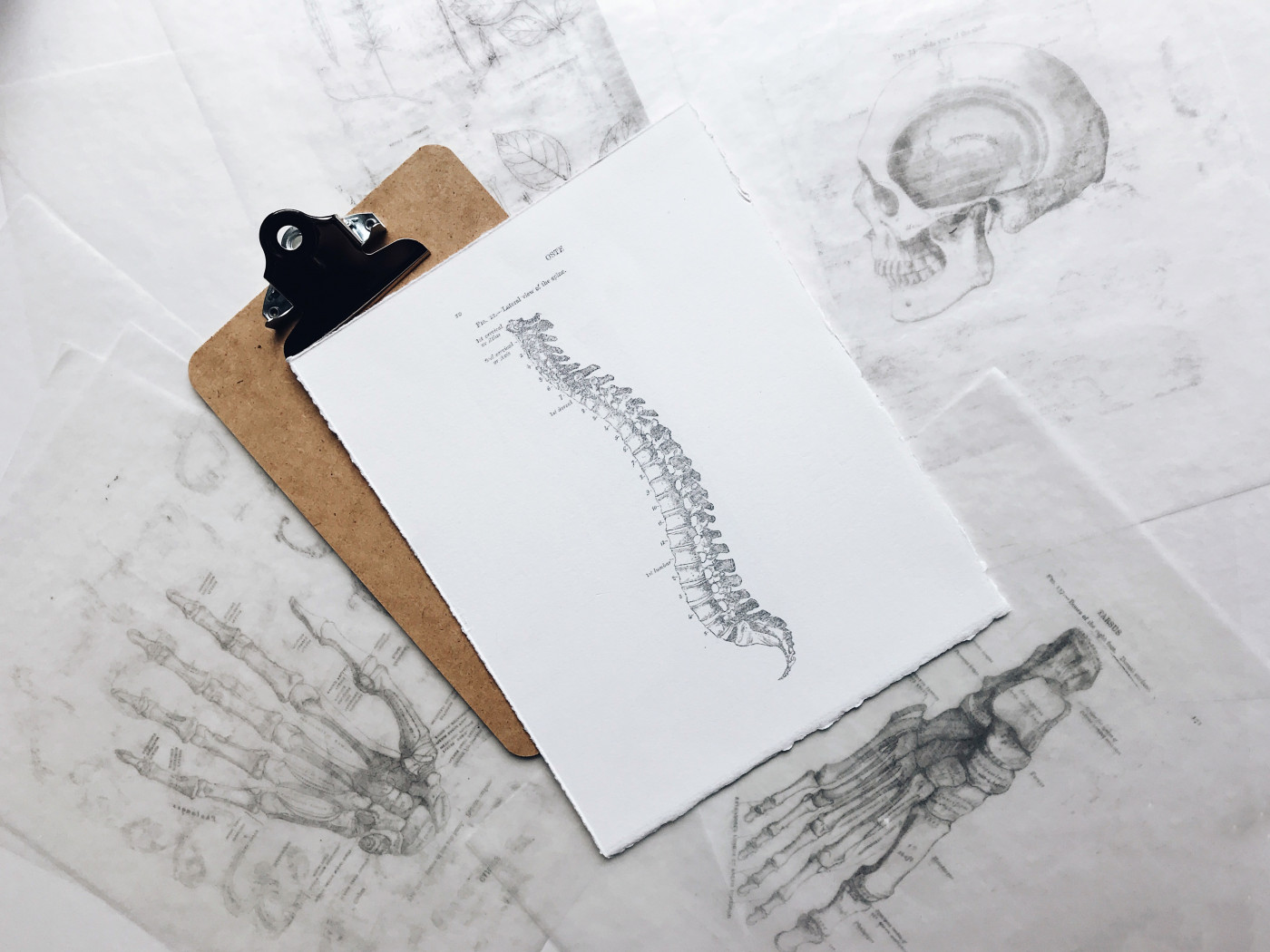
axSpA is characterized by chronic back pain and active inflammation of the sacroiliac joints (where the lower spine and pelvis connect). It’s known as ankylosing spondylitis (AS) when these changes can be seen on X-rays, and as non-radiographic (nr)-axSpA when no such damage is detected with this approach.
New spinal bone formation and bone resorption are hallmarks of the disease, suggesting altered bone metabolism. S100A4 is a protein that regulates cell growth and survival, and is associated with a number of conditions, including autoimmune diseases.
Research has shown that this protein represses bone formation, and its deficiency is associated with a lower number of osteoclasts — cells that break down bone tissue and regulate skeletal mass — and a higher number of active osteoblasts — the cells that form new bone tissue. The dynamic balance between the two cell types and their function is essential for healthy bone and joints.
As S100A4 is also involved in the Wnt signaling pathway, which maintains normal bone function, researchers in Czech Republic and Denmark evaluated the levels of the protein in axSpA and its association with disease severity, clinical profile, and formation of syndesmophytes — a type of bony growth forming inside a ligament and common in AS.
The study included 58 axSpA patients and 40 healthy controls. In the axSpA group, 21 patients (median age 30.6) had nr-axSpA, 17 (median age 31.6) had AS without spinal involvement (AS I), and 20 (median age 37.3) had AS with the presence of syndesmophytes (AS II) — indicating more bone formation.
Analysis of blood samples showed that levels of S100A4 were significantly higher in axSpA patients than in controls (317.0, compared with 89.7 ng/mL).
In addition, S100A4 levels were lower in AS II patients than in those with AS I. However, after adjustment for variables such as disease duration, age, and a marker of inflammation, the difference was no longer statistically significant. No differences were seen in protein levels between nr-axSpA and AS I patients.
Lower blood levels of S100A4 were associated with higher modified Stoke Ankylosing Spondylitis Spinal Score (mSASSS), which assesses damage seen in radiographs. Higher scores indicate more damage.
The researchers found that S100A4 levels were negatively correlated with disease duration, meaning that patients at early stages of the disease had higher levels of this protein than who had had it longer and had spinal involvement.
They also found that lower levels of S100A4 were associated with lower amounts of DKK-1, a protein that suppresses the Wnt signaling pathway and participates in the formation of syndesmophytes in AS. The association of between S100A4 and DKK-1 suggests that the two are co-regulated, the investigators said.
“Our results uncover the potential value of S100A4 and DKK-1 for assessing the syndesmophyte formation in axSpA,” they wrote. “However, larger and prospective studies are needed to further investigate the exact functional role of S100A4 in the molecular interplay underlying the bone metabolism and in the new bone formation in patients with axSpA.”
“S100A4 levels are elevated in patients with axSpA, particularly in those at early stages without the presence of syndesmophytes and may be involved in the altered bone formation,” the researchers said.